|
Diabetic retinopathy
Diabetic retinopathy is damage to the eye's retina that occurs with long-term diabetes. It is the leading cause of blindness in working-age Americans. People with both type 1 diabetes and type 2 diabetes are at risk for this condition.
There are two types, or stages of retinopathy:
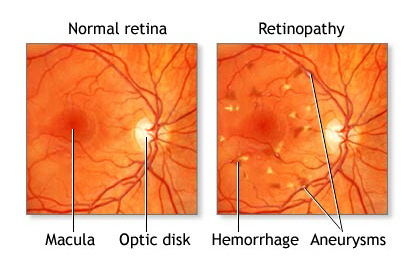
• Non-proliferative diabetic retinopathy develops first. Blood vessels in the eye become larger in certain spots (called microaneurysms) and may also get blocked. There may be small amounts of bleeding in the back of the eye, and fluid may leak into the retina. This can lead to noticeable problems with the eyesight.
• Proliferative retinopathy is the more advanced and severe form of the disease. New blood vessels start to grow in the eye. These new vessels are fragile and can bleed easily. Small scars develop, both on the retina and in other parts of the eye. The end result is severe vision loss.
Having poorly controlled diabetes for a longer period of time increases the chance of getting retinopathy.
Table1. Incidence of retinopathy relative to duration of Type I and Type II diabetes
Diabetes Type |
Duration of Disease |
Probability of Retinopathy |
Probability of Progression |
Type I |
10 years |
60 to 74% |
Unspecified |
Type I |
15 years |
98% |
25% proliferative retinopathy |
Type I |
20 years |
100% |
50% proliferative retinopathy |
Type II |
At diagnosis |
10 to 20% |
Unspecified |
Type II |
4 years |
4 to 29% |
Unspecified |
Type II |
15 years |
60 to 80% |
5 to 20% proliferative retinopathy |
Symptoms of diabetic retinopathy include:
• Blurred/hazy vision and you cannot focus
• Difficulty seeing at nighttime and in dim light
• Floaters
• Shadows or missing areas of vision
Most often, diabetic retinopathy has no symptoms until the damage to your eyes is severe. This is why everyone with diabetes should have regular eye exams.
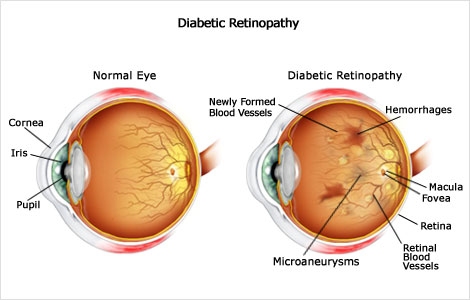
Other problems that may develop are:
• Macular edema when fluid leaks into this area, your vision becomes blurry
• Retinal detachment – a scarring may cause part of the retina to pull away from the back of your eyeball
• Glaucoma – an increased pressure in the eye may lead to glaucoma. If not treated, it can cause permanent blindness
• Cataracts formation
In nearly all cases, the eye doctor can diagnose diabetic retinopathy by dilating the pupils with eye drops and then carefully examining the retina.
The following are very important for preventing diabetic retinopathy:
• Tight control of blood sugar, blood pressure, and cholesterol
• Stopping smoking
• Lose excessive weight
People with non-proliferative diabetic retinopathy may not need treatment. However, they should be closely followed-up by an eye doctor trained to treat diabetic retinopathy. Most patients need a yearly eye exam.
Treatment usually does not reverse damage that has already occurred, but it can help keep the disease from getting worse. Once your eye doctor notices new blood vessels growing in your retina (neovascularization) or you develop macular edema, treatment is usually needed.
If you cannot see well:
• Make sure your home is safe so you do not fall
• Organize your home so that you can easily find what you need
• Get help to make sure you are taking your medicines correctly
• Cataract removal may be needed
Begin having eye examinations as follows:
• Children older than 10 years who have had diabetes for 3 - 5 years or more
• Adults and adolescents with type 2 diabetes ASAAP after initial diagnosis
• Adolescents and adults with type 1 diabetes within 5 years of diagnosis
Call for an appointment with an eye doctor if you have diabetes and you have not seen an ophthalmologist in the past year, if you are recently diagnosed with diabetes, or are planning to get pregnant. |